Most people think vapor therapy is harmless, but when you inhale aerosolized particles and chemicals they settle on your airway linings, altering mucus and cell function; you may experience short-term relief while your airways show inflammatory response and impaired cilia, and you are exposed to nicotine and toxic chemicals. Some studies find reduced exposure to combustion products compared with smoking, yet long-term effects on your lung repair and immunity are still being studied.
What is Vapor Therapy?
When you receive vapor therapy, you inhale an aerosolized mixture-steam, saline, medication, or oil droplets-that alters airway humidity and particle deposition; clinical aerosols are typically optimized to 1-5 µm so they reach bronchioles, while particles <1 µm or >5 µm behave differently and change efficacy and risk. You may benefit when humidity stays near 40-60%, but face harm if droplets carry lipids, contaminants, or toxicants that provoke inflammation.
Understanding Vapor Therapy
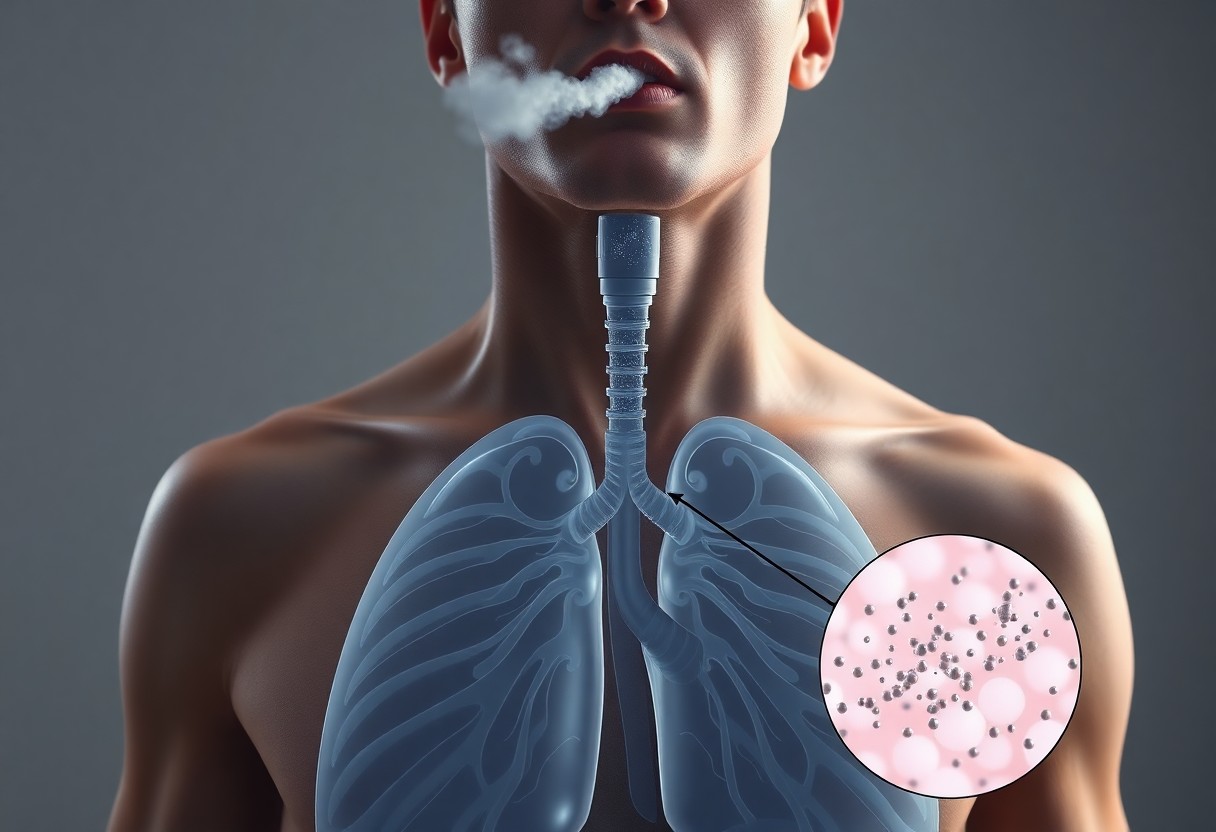
You should know aerosol physics determines where material lands: hygroscopic growth, Brownian motion, impaction and sedimentation shift particle fate. For example, droplets around 1-5 µm deposit in small airways, whereas 0.1-1 µm particles can reach alveoli; e-cigarette emissions often contain nanoparticles ~100-300 nm that can penetrate deep and enter circulation, raising inflammatory markers within hours in some studies.
Common Methods of Application
You’ll see several delivery approaches: medical nebulizers (jet, ultrasonic, mesh) producing mostly 1-5 µm therapeutic droplets; steam inhalation and household humidifiers that modify humidity; and e-cigarettes/vape devices creating ultrafine aerosols. Nebulizers can deliver drugs effectively, while vaping introduces <0.3 µm particles and chemical byproducts that pose lung injury risks.
Mesh nebulizers generally give higher lung deposition than jet types, so when you receive a bronchodilator (commonly salbutamol 2.5 mg), more drug reaches small airways. Steam above ~50°C risks scalding, and poorly cleaned humidifiers can aerosolize bacteria or fungi. During the 2019 EVALI outbreak, >2,800 people were hospitalized, showing How contaminated or chemically complex aerosols can cause severe, sometimes fatal, lung injury.
How Vapor Therapy Works
When you inhale e‑liquid aerosol, a coil heats propylene glycol and vegetable glycerin into a fine mist that carries nicotine and flavor chemicals; particles are typically submicron (often 100-300 nm), so they penetrate deep into airways. You get nicotine to your brain in roughly 10-20 seconds, producing rapid reinforcement. Some gains include fewer combustion products than cigarettes, but heating also forms carbonyls and other toxicants (The Truth About What Vaping Is Doing to Your Body).
The Science Behind Inhalation
As you inhale, aerosol physics and chemistry determine where particles deposit: larger droplets stick in upper airways, while submicron particles reach bronchioles and alveoli. Heating coils can exceed 200°C, creating carbonyls like formaldehyde at high power. You should note that nicotine salts boost blood levels at lower voltages, so device settings and e‑liquid concentration (commonly 0-60 mg/mL) strongly change systemic delivery and exposure.
Effects on Airways and Lungs
You often experience immediate airway responses: throat irritation, cough, and bronchoconstriction in susceptible people, plus measurable increases in airway inflammation markers. Clinical reports and imaging show airway hyperreactivity and inflammation, and the 2019 EVALI cases highlighted that additives (e.g., vitamin E acetate in THC products) can cause severe, sometimes fatal lung injury.
At the cellular level, studies reveal impaired mucociliary clearance, lipid‑laden macrophages, altered neutrophil function, and disrupted epithelial repair in both human bronchoscopy and animal models. You face reduced innate immunity and slower pathogen clearance after repeated exposure, which explains higher rates of respiratory infections and delayed recovery seen in several clinical and preclinical studies.
Benefits of Vapor Therapy
You can observe targeted airway effects when vapor delivers warm, humidified aerosol: medical nebulizers produce ~1-5 µm particles that reach lower airways, improving drug deposition and mucociliary clearance. Short sessions (5-15 minutes) often loosen sputum and ease breathing. At the same time, improper devices or additives can introduce toxicants or cause thermal injury, and clinical benefit hinges on device, particle size, and formulation.
Relief for Respiratory Conditions
You often get measurable symptom relief from vapor-delivered medications: nebulized bronchodilators like albuterol (typical 2.5 mg nebulized dose) and inhaled corticosteroid suspensions work best when aerosolized to ~1-5 µm, reaching bronchi to reduce bronchospasm and improve airflow in asthma and COPD. Nebulized saline helps mobilize secretions. Beware that vaporized additives or scented oils may provoke bronchospasm or allergic reactions in sensitive people.
Aromatherapy and Wellbeing
You may notice immediate sensory relief from aromatic vapors-eucalyptus (rich in 1,8‑cineole) and peppermint (menthol) stimulate nasal receptors and give perceived decongestion; menthol specifically activates TRPM8 to produce a cooling sensation. Short-term symptom relief is common, but long-term respiratory benefit is limited by evidence. Keep in mind imperative oils can irritate airways or trigger bronchoconstriction in reactive individuals.
You should consider delivery method: ultrasonic diffusers make larger droplets that linger in the nose and throat, while medical nebulizers create ~1-5 µm particles that can carry volatile compounds deeper. Small clinical trials suggest inhaled 1,8‑cineole may reduce cough perception, though results vary. Use diluted preparations, avoid heating unknown mixtures, and stop immediately if you experience wheeze, chest tightness, or irritation, since concentrated vapors can damage the airway lining.

Potential Risks and Considerations
Vapor therapy can relieve congestion but also carries risks: scald burns from hot water, aerosolized dispersal of microbes from poorly cleaned devices, and airway irritation from additives like menthol or crucial oils. Studies and reviews report limited evidence for reduced illness duration, while case reports tie oil-based inhalants to lipoid pneumonia. You should weigh small symptomatic gains against these documented hazards and device hygiene requirements.
Safety Concerns
Steam exposure can cause second-degree burns, especially when tents or bowls are used; several emergency departments report such injuries from home steam inhalation. Nebulizers vary in delivery-often only ~10-20% of a drug reaches the lungs-so dosing is inconsistent without medical guidance. Additionally, inhaled oils and unapproved additives have produced bronchospasm and inflammatory lung reactions in case studies, so you should avoid unregulated mixtures.
Who Should Avoid Vapor Therapy?
Children under 2, people with uncontrolled asthma or severe COPD, and immunocompromised individuals should generally avoid home vapor or steam therapies. Infants face high burn risk, asthma patients may experience bronchospasm from hot air or oils, and compromised immune systems increase danger from contaminated humidifiers that can aerosolize bacteria or fungi.
For example, household humidifiers have been linked in outbreak investigations to aerosolized Legionella and non-tuberculous mycobacteria, posing real infection risk for the immunosuppressed; pediatric burn units commonly treat toddlers scalded by bowls of hot water; and case series report asthma exacerbations after inhaling concentrated crucial oils-so if you fall into these groups, opt for saline-based nebulization under medical advice or consult your clinician before using vapor devices.
Comparing Vapor Therapy with Other Treatments
| Side‑by‑side overview of common airway treatments | |
| Vapor Therapy | Other Treatments |
| Mechanism: heats PG/VG or water to produce aerosol that deposits in upper/lower airways; particle size ~0.1-1 µm for e‑cig vapor. | Mechanism: inhalers/nebulizers deliver drugs (SABA, ICS) as 1-5 µm particles; systemic meds act via bloodstream. |
| Onset: fast symptomatic feeling; relief often <5-10 minutes for perceived ease of breathing. | Onset: SABA works in 5-15 minutes; nebulized antibiotics/steroids take longer but have proven clinical outcomes. |
| Evidence: limited RCTs for vapor as bronchodilator; concerns about long‑term airway inflammation and chemical exposure. | Evidence: multiple RCTs support ICS reducing exacerbations and bronchodilators improving airflow; risks include systemic steroid side effects. |
| Risks/uses: convenient for symptomatic relief but potential for airway irritation, nicotine dependence. | Risks/uses: targeted therapy for asthma/COPD with dose monitoring; antibiotics only for confirmed infections to avoid resistance. |
Traditional Medications
You’ll find short‑acting beta‑agonists (albuterol) give predictable bronchodilation within 5-15 minutes, while inhaled corticosteroids reduce exacerbations and inflammation over weeks; nebulizers and metered‑dose inhalers deliver 1-5 µm particles optimized for lower airway deposition. Systemic steroids are effective for severe flares but carry side effects like weight gain and hyperglycemia, so physicians reserve them for clear indications and monitor dosing closely.
Alternative Therapies
You may try saline irrigation, steam, or herbal inhalations for symptom relief; hypertonic saline (3%) nebulization is used in cystic fibrosis to improve mucus clearance, whereas evidence for steam or necessary oils is weak and some agents can trigger bronchospasm-avoid unregulated oils if you have reactive airways.
For more detail, clinical trials show nebulized hypertonic saline increases mucus hydration and expectoration in bronchiectasis and CF, and inhaled mannitol is approved in some regions to aid sputum clearance. Conversely, aromatherapy and steam lack robust RCT support and carry anecdotal risks; if you pursue alternatives, consult your clinician and use medical‑grade preparations to minimize the chance of airway irritation or allergic reactions.
User Experiences and Testimonials
When you read testimonials, you’ll see both quick symptom relief and safety warnings. Small surveys report 30-50% symptom relief after short vapor sessions, often linked to aerosol sizes that penetrate the airways. Some users describe scald burns or persistent throat irritation. You should weigh individual reports against device type, formulation, and measurable changes in coughing, mucus volume, and breathing effort.
Personal Stories
One teacher with seasonal congestion used a saline nebulizer (2 mL 0.9% NaCl, ~10 minutes) and noted improved breathing within 24 hours, showing how device and dose matter for you. Another person switched to homemade hot-water steam and suffered a second-degree burn after a spill, illustrating that technique and temperature directly affect your safety and outcomes.
Expert Opinions
Pulmonologists stress that particle size and formulation determine where aerosol deposits: 1-5 µm reaches lower airways, while oily or unregulated mixtures have case reports linking them to lipoid pneumonia. You should consult clinicians if you have asthma or COPD because experts note benefits are device- and dose-dependent and can vary widely between individuals.
Respiratory therapists commonly recommend medical nebulizers delivering 2-5 mL of 0.9% saline over 5-15 minutes to produce a consistent 1-5 µm aerosol; clinical studies and practice guidelines show this can improve mucociliary clearance and reduce work of breathing in some patients. They advise you not to add important oils or lipid-based substances, since those increase the risk of inflammatory lung reactions.
To wrap up
Upon reflecting, you see that vapor therapy mainly changes airway humidity and temperature, which can temporarily ease irritation and loosen mucus, but it can also deliver irritants depending on the device and substance used; weigh benefits against risks, follow safe practices, and consult a clinician if your symptoms persist or worsen.
FAQ
Q: What physiologic changes occur in the airways when you inhale warm, moist vapor?
A: Warm, humidified air increases airway surface liquid and can reduce mucus viscosity, which helps mucociliary transport. Heat and moisture also transiently increase blood flow to airway mucosa, which can relieve congestion and loosen secretions. In some people warm vapor produces mild bronchodilation through reflex mechanisms and by reducing airway surface tension, but the effect is short-lived and varies by individual and by underlying lung condition.
Q: Can vapor therapy meaningfully improve mucus clearance or shorten respiratory infections?
A: Vapor therapy can provide symptomatic relief-easier breathing, decreased nasal congestion, and improved expectoration-by hydrating secretions and supporting ciliary function. Clinical evidence shows symptom improvement for upper respiratory congestion but limited impact on the duration of viral infections. For thick bronchial secretions, medically directed humidification or aerosolized saline delivered by appropriate devices is more effective than brief home steam exposure.
Q: What are the main risks and safe-use considerations for vapor therapy?
A: Scald burns from hot water or steam are the most common danger; keep temperatures safe and avoid direct steam inhalation close to the face. People with reactive airways disease may experience bronchospasm with hot or cold vapors. Avoid inhaling unregulated aerosols, oil-based vapors, or additives (including important oils) because they can provoke inflammation or lipoid pneumonia. For chronic lung disease or uncertain symptoms, consult a clinician before using home vapor treatments; medically prescribed humidification or nebulized medications should be used under guidance.
Medical Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider before starting, stopping, or changing any treatment, especially if you are pregnant, nursing, have a medical condition, or are taking medications. Never disregard professional medical advice or delay seeking it because of something you have read here. If you experience severe symptoms, allergic reactions, or think you may have a medical emergency, seek immediate care.


